Anxiety is a natural alarm system that helps us prepare for threats. But when the worry switch gets stuck in the “on” position—intruding into work, relationships, sleep, and health—we move beyond everyday stress into Generalized Anxiety Disorder (GAD). People with GAD often describe a constant, hard-to-control stream of “what if?” thoughts paired with body sensations like tight muscles, a fluttering chest, stomach discomfort, or restless sleep. This comprehensive guide explains what GAD is (and isn’t), how to recognize the signs, how clinicians diagnose it, and which treatments have the strongest evidence—from cognitive behavioral therapy to medication and lifestyle approaches. You’ll also find practical techniques you can use today and clear guidance on when to seek professional help.
Important: This article is educational and not a substitute for medical advice. If anxiety is disrupting your life, speak with a licensed mental health professional or your physician.
What Is Generalized Anxiety Disorder (GAD)?
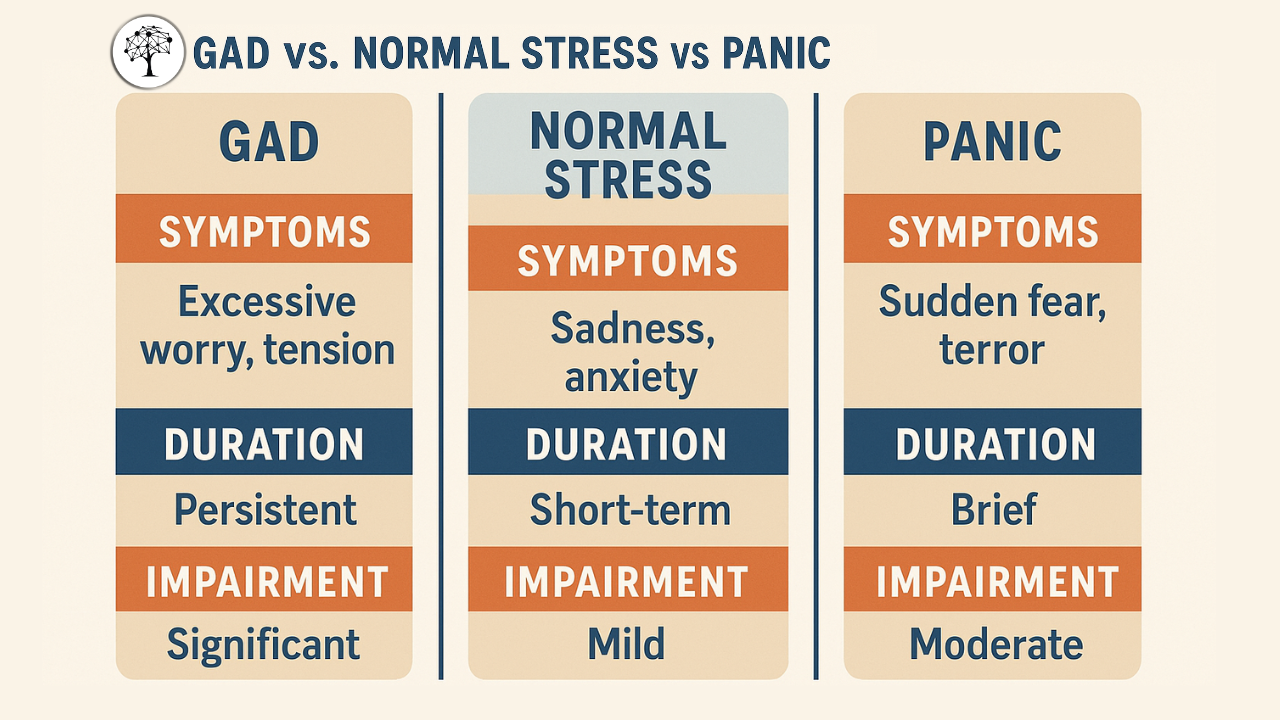
GAD is a chronic pattern of excessive, hard-to-control worry about multiple life areas (work, health, finances, family, safety) on more days than not for at least six months, accompanied by physical and cognitive symptoms such as restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbance. Unlike phobias (which center on a specific trigger) or panic disorder (sudden surges of intense fear), GAD is diffuse and persistent—the theme of the worry can shift, but the anxious “tone” remains.
The difference between stress, worry, and GAD
Stress is a response to external demands (deadlines, conflicts). It usually subsides once the situation resolves.
Worry is a mental problem-solving attempt—useful in short doses.
GAD involves excessive, uncontrollable worry that is out of proportion to the situation, continues even when things are going well, and impairs functioning.
Common cognitive patterns in GAD
Intolerance of uncertainty: Needing absolute certainty before feeling okay.
Catastrophizing: Assuming the worst is not only likely but imminent.
Over-responsibility: Believing one must prevent every possible bad outcome.
Thought-action fusion: Feeling that thinking about something makes it more likely.
How GAD shows up in the body (somatic symptoms)
Muscle tension, jaw clenching, or shoulder/neck pain
Restlessness or feeling “keyed up”
Headaches, lightheadedness, or chest tightness
Gastrointestinal discomfort (butterflies, nausea, IBS-like symptoms)
Sleep difficulties (long sleep latency, frequent awakenings)
Increased startle response, sweating, trembling
Risk factors and maintaining loops
Early experiences: Childhood adversity, loss, or chronic stress can sensitize threat systems.
Temperament: Higher trait neuroticism and behavioral inhibition.
Cognitive styles: Habitual rumination, all-or-nothing thinking, reassurance seeking.
Behavioral cycles: Avoidance reduces anxiety short-term but keeps it going long-term by teaching your brain that normal uncertainty equals danger.
Recognizing Symptoms and Getting a Diagnosis
A GAD diagnosis is clinical (based on a structured interview), not a lab test. The key elements are duration, severity, impairment, and exclusion of other causes.
Core psychological symptoms
Persistent, excessive worry across domains (work, health, family, finances)
Worry feels difficult to control; attempts to stop it backfire
Intrusive “what-if” scenarios; difficulty concentrating; mental fatigue
Irritability, impatience, and perfectionism that slow decisions
Core physical symptoms
Muscle tension; headaches; trembling; sweating
Palpitations or chest tightness (non-cardiac)
GI symptoms; dry mouth
Sleep problems (trouble falling asleep, non-restorative sleep)
Functional impact
Procrastination, over-checking, or avoiding tasks
Reassurance loops (asking others repeatedly for certainty)
Withdrawing from social or professional opportunities
Reduced productivity and quality of life
Differential diagnosis and comorbidity
GAD commonly co-occurs with depression, social anxiety, panic disorder, and substance use. Medical conditions (thyroid issues, anemia, cardiac arrhythmias), medications (stimulants, some decongestants), and caffeine can masquerade as anxiety. A clinician will assess these to ensure the right plan.
When to seek help
Worry lasts 6+ months and is hard to control
You’re canceling plans, underperforming, or losing sleep regularly
You feel on edge most days or use alcohol/cannabis to cope
You have thoughts of hopelessness or self-harm—seek urgent care immediately
Evidence-Based Treatments That Work
Good news: GAD is highly treatable. Treatments often combine psychotherapy, medication, and skills practice that retrain the brain’s alarm system.
Cognitive Behavioral Therapy (CBT)
CBT is first-line for GAD. It targets the cycle of worry, avoidance, and reassurance seeking.
Key CBT components
Psychoeducation: Understanding how worry is maintained reduces shame and increases motivation.
Cognitive restructuring: Spotting catastrophizing and replacing it with balanced thinking (not “positive thinking,” but probability-based thinking).
Worry time: Scheduling a 20-minute daily window to postpone and contain worry, preventing all-day rumination.
Exposure to uncertainty: Gradual, repeated practice doing things without certainty (sending the email without triple-checking) to prove safety to your nervous system.
Behavioral activation: Re-engaging with meaningful activities even when anxious; action first, motivation later.
Relapse prevention: Building a plan to maintain gains, including early-warning signs and coping scripts.
Acceptance and Commitment Therapy (ACT)
ACT helps you make room for anxious sensations and refocus on values. You learn mindfulness skills (defusion, present-moment awareness) and values-driven commitments so anxiety is not the boss of what you do.
Intolerance of Uncertainty (IU) Training & Metacognitive Therapy
If your anxiety is fueled by “I must be 100% sure,” IU-focused protocols and metacognitive therapy reduce the need to control thoughts and help you change your relationship to worry.
Medication Options (discuss with a prescriber)
SSRIs/SNRIs (e.g., sertraline, escitalopram, venlafaxine, duloxetine) are commonly first-line. They reduce baseline anxiety over weeks.
Buspirone may help with chronic worry and is typically non-sedating.
Pregabalin can be considered in some cases.
Benzodiazepines (e.g., lorazepam) may relieve acute anxiety but carry risks (tolerance, dependence, sedation) and are not first-line for long-term management.
Beta-blockers may help performance situations (e.g., presentations) by reducing physical arousal.
Medication decisions are individualized. Never start/stop a medication without professional guidance.
Lifestyle and Self-Help That Amplify Treatment
Sleep hygiene: Fixed wake time; limit late caffeine; buffer time before bed; dim light.
Exercise: 150+ minutes/week moderate activity; even short daily walks reduce baseline arousal.
Breath training: Slow diaphragmatic breathing (inhale ~4, exhale ~6–8) 5 minutes, 2–3×/day.
Mindfulness “noting”: Label thoughts as “planning,” “worrying,” or “remembering” to reduce fusion.
Limit reassurance: Agree with a partner on once-and-done answers.
Reduce safety behaviors: Send the message after one check; attend the event without an exit plan; leave the phone in another room for 30 minutes.
Caffeine/nicotine awareness: Track intake and test reductions; consider a 2-week caffeine holiday if jittery.
Nutrition & gut comfort: Regular meals with protein/fiber; notice foods that aggravate GI symptoms.
Digital boundaries: News/social media windows; do not graze on headlines all day.
A 2-Week Starter Plan (you can begin today)
Days 1–3
Track triggers, worries, and safety behaviors.
Start box breathing (4–4–4–4) or paced breathing twice daily.
Pick one avoidance to reverse (e.g., open unread emails).
Days 4–7
Create a 20-minute worry window; postpone worries until then.
Do the feared action with one check, not three.
Walk 20 minutes daily, outside if possible.
Days 8–14
Add values actions (call a friend, apply to a role, schedule a class).
Practice uncertainty exposures: send a message with a minor typo, try a new route without pre-mapping every turn.
Review progress; book a therapy consult if impairment remains high.
Short Checklist (for readers to screenshot)
Worry most days for 6+ months about multiple topics
At least three symptoms (restless, fatigued, tense muscles, poor sleep, irritability, poor focus)
Impairment at work/school or in relationships
Started a daily worry window (postpone worries)
Practiced paced breathing 5 minutes, 2–3×/day
Scheduled one uncertainty exposure today
Prioritized sleep: fixed wake time + buffer before bed
Booked a consult with a licensed professional if symptoms persist or worsen
Final Tip
Anxiety shrinks your life by promising safety in exchange for avoidance. The paradox is that confidence grows by acting while anxious, not by waiting to feel fearless. Small, repeatable steps—paired with evidence-based treatment—are how GAD becomes manageable, then optional.
Frequently Asked Questions
What is GAD?
A long-lasting pattern of excessive, hard-to-control worry across life areas, with physical symptoms like muscle tension and sleep problems, that impairs daily functioning.
How is GAD treated? Can GAD go away?
First-line options include CBT (skills for worry and uncertainty), SSRIs/SNRIs or buspirone, and lifestyle strategies (sleep, exercise, breath training, mindfulness).
With the right combination of therapy, skills practice, and (if needed) medication, many people experience major relief and sustained improvement.
What’s the difference between GAD and normal stress?
Stress ends when the trigger passes. GAD persists, shifts topics, feels uncontrollable, and disrupts work, relationships, and sleep.